Stopping Gout Together › Forums › Help My Gout! The Gout Forum › Three Stage Gout Pain Prevention Plan
- This topic has 24 replies, 7 voices, and was last updated 4 years, 3 months ago by
nobody.
-
AuthorPosts
-
-
March 19, 2017 at 1:12 am #4329
d q
Participant
@Keith , I noticed you have a three stage plan for dealing with acute flares and I was wondering what you use for each, so for example lets say someone gets an acute flare today; what would be your dosing to hit hard?
From what I understand you would use a combination of the below or if the pain is really bad all three together:
Colchicine 0.5mg twice a day – how many hours apart?
NSAID – Which specific ones and at what dosing?
Paracetamol – Do you take this simultaneously with the above two or later?That way the thread can be quickly accessible and help members better understand immediate therapy.
Thanks 🙂
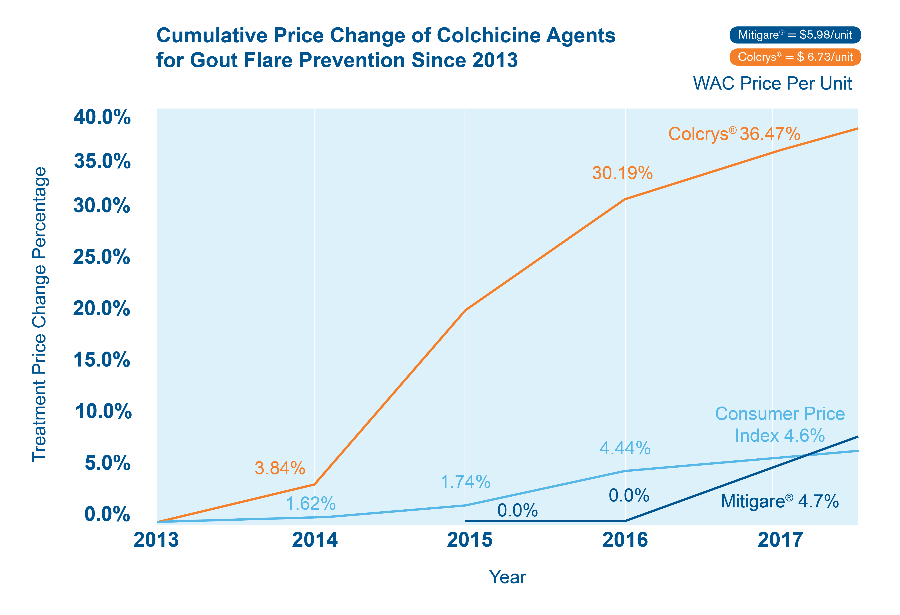
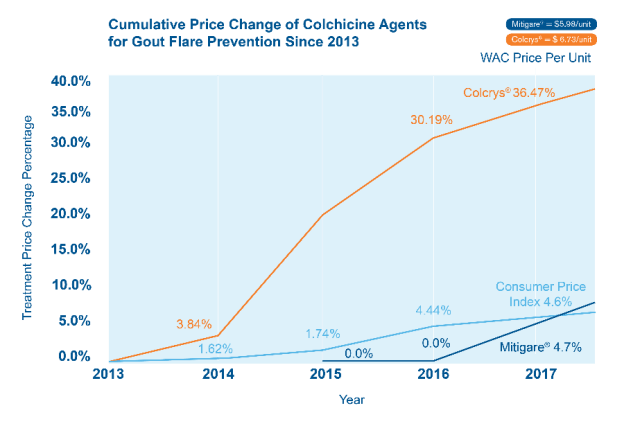
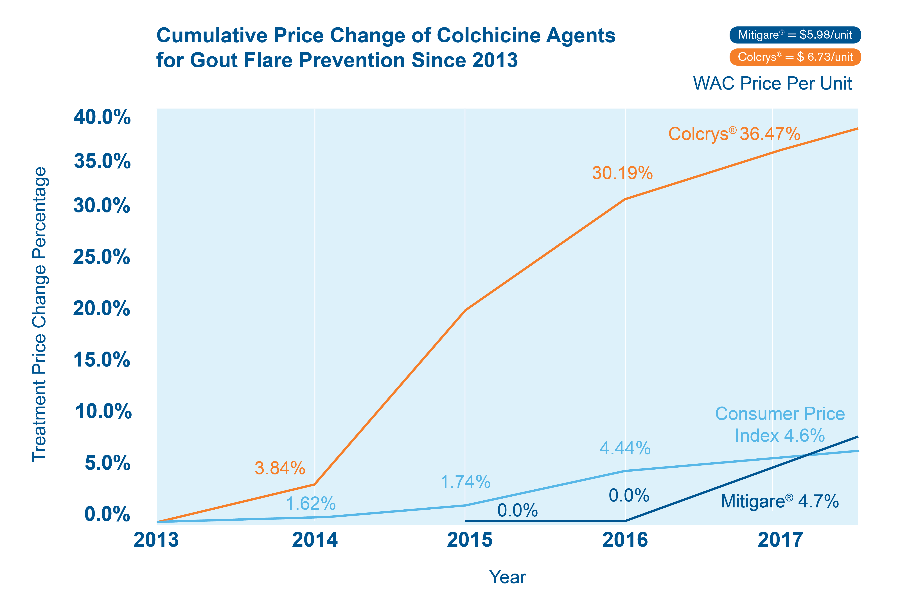
Mitigare is a brand of Colchicine just like Colcry$ but cheaper
-
March 19, 2017 at 1:12 am #2827
Gout Patient
ParticipantGout Necessities: Mitigare cheaper than Colcrys
I was misdiagnosed several times with gout. Many trips to the ER that were either a sprained ankle or sprained toe. I will keep this short and sweet. If you have gout the necessities are Mitigare, (brand name of colchicine) as my insurance will not cover colchicine or Colcrys. Methylprednisolone Steroid pack. This will stop gout in in tracks. For me, it was within 8 hours. I have started on Allopurinol 300mg per day and have not experienced any gout symptoms at all or any side effects, regardless of diet or alcohol intake.
I would recommend you keep these drugs on hand so that you are not immobilized or wheeling yourself around in your office chair or crawling on the floor because you cannot walk. Which I have done many times.
Don’t needlessly suffer, my final gout attack put me down for 3 weeks and I thank the folks at the ER and my doctor for treating me with the correct drugs, and having prescriptions on hand so that I don’t needlessly suffer! It has been a God Send.
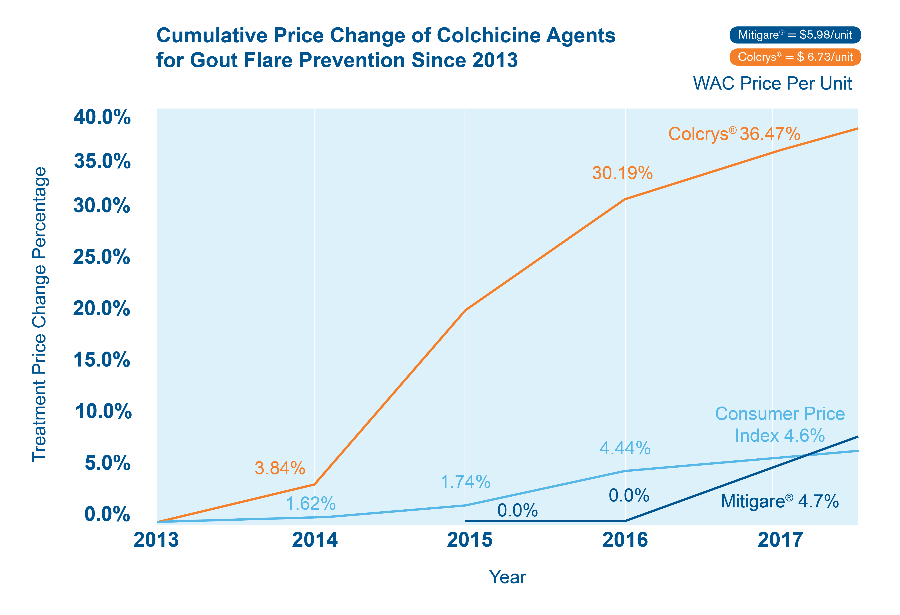
Mitigare is a brand of Colchicine just like Colcry$ but cheaper
Pain relief is a necessity for gout sufferers. Colchicine is best but Colcrys is expensive. Get Mitigare – the same gout drug. Now pay less for colchicine.
-
March 19, 2017 at 10:23 pm #2850
 Keith TaylorParticipant
Keith TaylorParticipantIt’s good to see that Mitigare is finally getting recognized more. It’s a licensed brand of colchicine that’s cheaper than Colcrys. If more gout sufferers bought it, it might bring down the cost of Colcrys. I wrote about Mitigare last year.
-
-
June 22, 2017 at 2:58 pm #4349
Patrick
Participantd q,
Hey buddy. I’ve used that 3 step plan before, but I include a 4th step and it works for me. I have always preached the benefits of Methylprednisone (Z pack). I keep one with me at all times, just in case. It’s a 6 day, progressive antibiotic, that I find if taken at the first onset of gout pain, flood the body with Methylprednisone and it’s gone. Early.
Some won’t (or can’t) take it. I understand that. It works for me, so when I used to get acute flares, I’d hit the pain with a mass dose of Methylprednisone (4 tablets immediately, then (2) 4 hours later), 2 Colchicine tabs, and 2 Naproxen (Pharmacy grade) along with my Allopurinol dose. That was my formula, but knock on wood, I haven’t had to do it in over 18 months……and counting.
Hope all is well my friend.
-
June 24, 2017 at 11:42 pm #4379
d q
ParticipantHey Patrick pal, I’m doing good, I know your having a difficult time, how is it all going back home?
I’m definitely going to discuss Methylprednisone option with my new rheumatologist and see if it’s safe for me to use and if he can prescribe it. Is it common to take with accute attacks?
With regards to colchicine, how many hours apart did you use to wait between each dose (it was 500micrograms right)? Did you continue the colchicine and naproxen alongside the 6 day course of Methylprednisone or stop those earlier or later?
Thanks buddy.
@Keith – what about you mate? -
June 26, 2017 at 5:21 am #4394
Patrick
Participantd q,
All is going as good as I expected on the home front. My fathers issue is terminal, so we just wait…
To your questions…Methylprednisone is ONLY taken during an acute attack. As soon as the attack starts, you start the 6 pill (day 1) dose. I would normally take 4 as soon as I felt pain, then the remaining 2 about 8 hours later. Then 5 the next day, then 4, then 3 and so on until you are done in 6 days. Usually after the first day, the pain is gone but you MUST finish the 6 day pack.
I took Colchincine in conjunction with the Z-pack and Naproxen. My dose was 0.6 mgs. I would take 2 to start, then 2 more 8 hours later. That was my plan and it worked for me. Consult your Rhuemotologist of course, before you start this plan.
-
June 26, 2017 at 11:09 am #4401
 Keith TaylorParticipant
Keith TaylorParticipantHi, d_q, nice to see more interesting questions.
The thing about my three-pronged gout pain attack plan is that it’s mine. Because, if there is only one thing you are ever allowed to remember about gout treatment it’s: “Treat To Individual Target”. So, my personal plan is actually at Acute Gout Attack Treatment Plan. But, there are many individual points to discuss how that would apply to anyone else.
Therefore, I don’t want to post it as a “quickly accessible thread”. Because I feel it should be a slowly ingested example of a plan. Then, other gout patients can inspect each point to see how it applies to them. Unfortunately, that’s a longwinded process. So, doctors have to rely on standards that have served them through their careers. Because sometimes you have to accept “average” treatment if there are only 10-15 minutes available.
Otherwise, nothing would ever get prescribed. But in this gout forum, we can guide patients through the process.
Firstly, we have to understand individual attitudes to pain. Because pains that might be tolerated by one person will put another in bed. This is important because, in my experience, immobility tends to extend the duration of a gout flare. But, I have not yet found science to support this in the general gout population.
Next, we consider each of the points:
1. Inhibit Inflammation.
2. Reduce Inflammation.
3. Block Residual Pain.1. Colchicine. To answer your initial question, I’d suggest one colchicine at night. Then another in the morning, as required. But, that might not fit an individual’s lifestyle. Also, there’s evidence to suggest it’s not always the most appropriate dose. So, at best it’s a starting point for a discussion between doctor and patient. Ultimately, all I’m really trying to do is support gout patients so they ask the right questions and understand their doctor’s responses.
On the other hand, colchicine might be totally inappropriate for some patients. Because it suppresses the immune system. So, depending on personal circumstances it can be a very bad idea.
2. We can see here, there are opposing views on NSAIDs and steroids. Some think that the immunosuppressive nature of drugs like methylprednisolone, methylprednisone, and corticosterone can support or replace colchicine for gout. Others, like me, would never consider them. In any case, we cannot give general guidance for specific NSAID choice or dosing. Because that’s the doctor’s job.
Anyway, all NSAIDs are medically similar. So, most doctors will just prescribe the one they are most used to. Then, if a patient doesn’t get on with it, they might try a different one. For example, ibuprofen, naproxen, and indomethacin are common choices. But even though one might seem better tolerated than another, they all have bad cardiac risks after long periods of high doses.
3. I’ve heard 2 arguments about paracetamol dosing as an addition to NSAIDs. I was taught to intersperse the dose. That is, NSAID at every 4 hours starting at zero hours. With paracetamol every 4 hours starting after 2 hours.
But a friend, whose extreme pain experiences are different from mine, recommends taking them together. “Because they work differently, so provide more pain relief when taken at the same time”. Anyway, I think this goes back to being mindful about your pain symptoms, and the effects of treatment. Then, you can adjust dosing to suit your situation.Always remember, doctors will suggest dose intervals based on average half-life and other factors. But, within drug safety limits, there is a great deal of flexibility.
To summarize, I hope you can see why doctors often prescribe a “one-size-fits-all” treatment plan. Because they simply do not have time to discuss all these different aspects. Also, in most cases, the patient gets the pain relief they want. So, it’s only worth discussing individual cases when there is a specific problem. In that case, the starting point is almost certainly different from my Acute Gout Attack Treatment Plan. And, the problems are always unique.
Finally, to answer your question “someone gets an acute flare today; what would be your dosing to hit hard?”
Dear Someone (related to nobody?),
Ask your doctor if the following is safe given your medical history:
1. Take 2 colchicine immediately (for 0.5mg or 0.6mg pills) with the maximum dose of ibuprofen. Try to keep affected joint moving.
2. At 2 hours, if symptoms persist, take another colchicine with maximum dose paracetamol (acetaminophen). Try harder to keep affected joint moving.
3. At 4-5 hours, repeat ibuprofen. Are you really trying to keep moving? Note that I’ve considered increasing the interval if symptoms are more tolerable. Sometimes I consider reducing the dose.
4. At 6-8 hours, repeat paracetamol. Accept you’re a wimp when it comes to pain tolerance.
If your doctor is concerned about any aspect of this emergency gout flare treatment, let’s discuss how we can improve it just for you.Yours with love, tolerance, and patience.
KeithI wonder if anyone kept reading long enough to read the final answer?
There is a standard colchicine dose for gout. But be flexible depending on your plan and your symptoms.
-
July 13, 2017 at 4:44 pm #4614
d q
Participant@Keith – hello mate, you know me.. Always trying to educate myself and others where possible 🙂
Fantastic comprehensive response. Thanks 🙂
You raise interesting points particularly with;
1. immobility and it extending the duration of the gout flare – Whilst this may be true I do feel it may delay the healing time. Since my last flare I’ve kept as mobile as possible but I notice after a long days movement my gout flare foot starts to hurt and the pain increases further as I exert further mobility. Not exercise just walking. That was certainly not the case with my previous two attacks. But that could all be down to this attack being invoked by allopurinol.2. You mention one Colchicine at night and one in the morning (two a day)? I’m not too sure I understand as further down you mention two tablets and one an hour later (3 a day). Is the first option what you generally would take if you got an attack and the second a general dose?
3. Finally during an accute flare how many days do you generally take the Colchicine for?
Thanks mate.
-
July 18, 2017 at 10:57 pm #4678
-
July 19, 2017 at 6:01 am #4679
 Keith TaylorParticipant
Keith TaylorParticipant1. Sorry d_q, that’s all a bit too general. I need a timeline of walking and pain meds to understand your symptoms in relation to pain meds. Can you give me an hour-by-hour list of symptoms, meds, and exercise?
2. I keep getting 2 maximum a day wrong. Because it’s actually max of 3 colchicine tabs per day unless they are 1mg tablets. Even then, individual cases might warrant more. But personally, I’ve never taken more than 2 per day (0.5mg). Or, had the need to.
I’m putting the discrepancies down to lack of distinguishing between preventative colchicine and “as required”. In future, I’ll try to take more care. But, in my defense, most of my lack of focus is down to analyzing what-if scenarios. I’m usually better when I’m discussing this in an actual one-on-one situation.3. Until you feel the need to stop.
I feel like I’m getting an education here on taking more time to vet questions before I make assumptions and spout advice that might be too general. So, I need to emphasize there is no right way to take colchicine. There are certainly wrong ways because too much of this poison is fatal. But the right way is more about understanding what is going on in your body, from day-to-day and during the day.
Personally, I try to be acutely aware of symptoms and how they are progressing. Because it’s better to adjust gout pain medicine on an hour-by-hour assessment rather than blindly rely on x number of pills per day.
Finally, if you are concerned about taking colchicine, I would always advise not taking it. Why burden yourself with the anxiety of drugs you don’t want to take when there are alternatives for gout pain control?
To explain, we are discussing the 1st stage of a 3 stage gout pain prevention plan. Which means stopping, or limiting, inflammation from getting worse. So, the choice is colchicine, steroids, or nothing. Personally, I will only take steroids if a doctor forces them on me when I’m unconscious. But, other people love them. Again, personally, I went many many years with adequate pain control from ibuprofen and paracetamol. I just found colchicine added speed and convenience to the mix. Also, I’m concerned about the long-term effects of high dose NSAIDs. But, I’m perfectly happy with low dose colchicine.
Anyway, that’s enough of my rambling for now. But, I’ll probably add lots more once you reply about Q1.
-
July 24, 2017 at 12:11 am #4735
d q
Participant@Keith – Hello mate, thanks for getting back to me.
1. I’ll fire up a separate thread for this point as I feel it would provide us both with greater granularity.
2. Just so I understand your answer about the colchicine a little better. So you don’t or didn’t really use strong NSAIDs like naproxen or diclofenac and instead used ibuprofen and paracetamol with colchicine for accute attacks?
The reason I ask is on the arthritis research UK website (http://www.arthritisresearchuk.org/arthritis-information/conditions/gout/treatments.aspx) it says NSAIDs with colchicine shouldn’t be taken? Unless I’m understanding your previous post (#4401) incorrectly and ibuprofen isn’t really considered a strong NSAID?
P.s. Would two colchicine tablets you take when you used to get an accute flare be an hour apart or would they be 12 hours apart (morning / evening)?
3. Would that be the same approach as naproxen? Continue to use for two days after symptoms have subsided?
Thanks Keith 🙂
-
July 25, 2017 at 7:04 am #4800
 Keith TaylorParticipant
Keith TaylorParticipant1. Looking forward to it.
3. Yes, but personally I stop any gout pain relief the moment the pain becomes tolerable. I include colchicine in that. Because it contributes to the gout relief package without actually relieving pain.Now the biggie.
2. I’ve never been aware that one NSAID is stronger than another. I naively assumed that a dose dependent amount of gout pain relief was available from any NSAID. Also that the choice was down to personal tolerability and preference.
I’ve never had any problems at all with ibuprofen. So, I’ve never felt the need to risk anything else. But, for completeness of my knowledge, I’d love to see some references to pain relief comparatives between different NSAIDs. Please share some links.
Speaking of link sharing, I hope they are better than the Arthritis Research UK link. Because they spend over £4m annually on “Information and Awareness” (2015/16 accounts). So, you’d think they could do a better job.
To clarify:
– Uric acid lowering section gives no explanation of debulking. Also, it is confused by a pointless reference to high purine foods that makes no distinction between food from plant and animal.
– Ice pack suggested with no reference to warming joints after ice pack application. Or, just using a warm compress.More importantly, we are talking about colchicine:
So, where the F has “You shouldn’t take colchicine at the same time as NSAIDs” come from?
– The big seller, Colcry$ (due to Americans loving their insurers spending too much money) has no mention of NSAIDs.
– What should be the biggest seller, Mitigare (due to it being a very affordable alternative to Colcry$) has no mention of NSAIDs. Both Mitigare and Colcry$ warn against use in conjunction with drugs that inhibit both P-gp and CYP3A4.
– A UK colchicine provider, Wockhardt/CP Pharmaceuticals Ltd (who provided the colchicine that my doctor prescribed alongside ibuprofen) has no mention of NSAIDs. But, it does have a completely different list of other medicines, compared to Mitigare and its expensive cousin.
And, finally…
Australian Rheumatology Association provides a free fact sheet on colchicine (brands Colgout & Lengout) which includes:Colchicine may be taken if needed in combination with other arthritis medicines, including […] anti-inflammatory medicines (NSAIDs) such as naproxen (Naprosyn) or ibuprofen (Brufen/Nurofen)
Interestingly, the Colgout label does warn against combining NSAIDs and colchicine in patients with stomach problems. So, it might be better to try them individually at first. Then, combine if no stomach problems. Personally, I’ve been medically described as having a “cast iron stomach”. Because I’ve never had any ibuprofen problems, even at the maximum prescribed dose.
The Lengout label looks very similar to Colgout. But, I haven’t done a complete comparison. Notably, both these Australian colchicine brands have a comprehensive list of other medicines to avoid at the same time as colchicine. Also, they indicate that colchicine should only be taken if NSAIDs can’t be tolerated or don’t work. So, this suggests an “either/or” approach instead of my beloved combination. Which kind of supports my other main tenet:
Gout pain relief combinations must be developed by doctor and patient working together for the patient’s best interest at the time of treatment
-
-
July 27, 2017 at 11:10 pm #4823
d q
Participant@keith – thanks for the detailed response mate.
3. Yes, me too. My pain tolerance is generally quiet high but when it comes to a gout flare I think even the slightest feeling of pain warrants immediate treatment to prevent it getting worse and stop it in its tracks.
2. I guess that ibuprofen being available without prescription even if one intends to take the maximum dose gives the impression that it isn’t as strong as naproxen, diclofenac, etc. So your approach in using a milder NSAID such as ibuprofen is definitely the wiser one. One could argue that you can take a lower dose of naproxen but then it being still prescription only leads me to believe it’s best to try and stick with ibuprofen first.
It’s a little strange that no clear information is available on the matter of NSAID’s with Colchicine. I mean if it can provide effective relief with no major side effects then it should generally be prescribed to help patience get better quicker.
Just to confirm, was your three stage pain prevention plan devised with your rheumatologist or did you do your own research and try it yourself and find it to be safe?
Finally, those two colchicine tablets you take when you used to get an accute flares, would they be an hour apart (one then the second an hour later) or would they be around 12 hours apart (morning / evening)?
Thanks Keith
-
July 30, 2017 at 2:50 pm #4854
d q
Participant@Keith – hope your well pal. Just a bump on this when you have time (specifically the last part) cheers 🙂
-
July 31, 2017 at 2:56 pm #4860
 GoutPal HelpDeskParticipant
GoutPal HelpDeskParticipantSorry, d_q, I’m slow in replying at the moment. Because I’m having to do the maintenance here (@ goutpal – deliberate space to stop me emailing myself). So, @ keith responses have to come second, until I catch up.
Anyway, once I get caught up with the backlog, I will summarize all the points here. Because I’m losing the context. So, I fear if I just fire off a few answers without reviewing the whole topic, I might easily contradict myself.
Please feel free to bump it again if you get fed up of waiting.
Cheers
Keith
-
-
July 31, 2017 at 8:39 pm #4891
d q
Participant@Keith – no worries mate, totally understand. Take your time.
p.s.
When you’ve got a minute, I’m really curios, those two colchicine tablets you took when you use to get accute flares, would they be an hour apart (one then the second an hour later) or would they be around 12 hours apart (morning / evening)?Thanks buddy
-
August 1, 2017 at 5:57 am #4897
 Keith TaylorParticipant
Keith TaylorParticipant@d_q
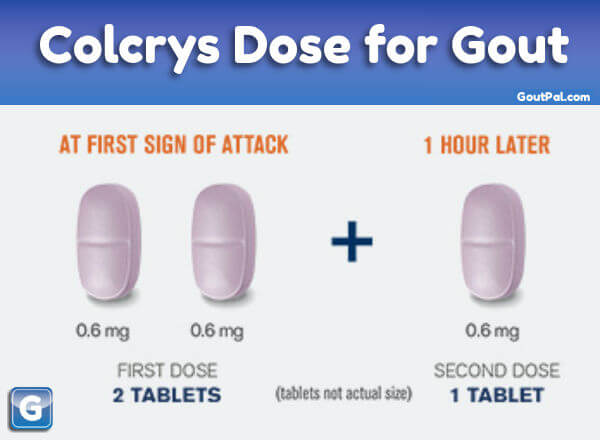
KQ1. Where does the 1-hour colchicine dose interval come from? Is it the Colcry$ picture I used to illustrate an earlier reply? If so, I hope you realize they are robbing bastards, and not to be trusted? On the other hand, I’ll recheck their research as part of my aforementioned review of this thread. Because that should indicate if it’s a medical optimal dosing regime. Or, as I strongly suspect, an accountant’s optimal profit dose. Interestingly, I thought I’d invented spelling Colcry$ with a $. But my spell checker (the exceptionally good Grammarly) recognizes it just fine. 🙂
KQ2. Where does the 12-hour colchicine dose interval come from? You’ve mentioned it 3 times now without explaining where it comes from.
KQ3. Why do I only get 2 choices of colchicine dose interval?
-
August 1, 2017 at 6:12 am #4898
 Keith TaylorParticipant
Keith TaylorParticipant@d_q, I’ve been thinking during my coffee break. Because, when I see things more complicated than a simple question and answer, I automatically move to 7-Step Progress mode. Then, I go back to the beginning and recheck what we are trying to achieve.
So, I started a quick review, and the lack of purpose is hitting me straight between the eyes. I think that is my fault, with hindsight. Because I should have asked for clarification as my first response.
To explain, I get the feeling you are looking for a one-size-fits all Three Stage Gout Pain Prevention Plan. But, that is not how I work. Because all aspects of gout management need to apply general principles to individual needs. Therefore, I want to take a common plan. For example, the Colchicine-NSAIDs-Paracetamol plan you started with. Then highlight for individual gout patients which points they need to make decisions on.
In that way, I can present an annotated plan that highlights personal choice. Together with guidance where they might make choices, discuss with their doctor, or seek extra info.
But, if I’ve read this wrong, maybe you are seeking your own personal acute gout pain plan?
So, d_q, can we restart by clarifying what we are hoping to achieve here? Then, I can summarize progress so far in the right context.
-
-
August 1, 2017 at 11:40 pm #4900
d q
Participant@Keith – thanks for your response mate.
I think there’s a slight confusion. I was just asking about your three stage prevention plan. I’ll start a separate thread for us to discuss one for me.
My question about colchicine was referring to an earlier thread here where you mentioned you take two tablets and no more then 1mg per day because you’ve never needed to. My question was how many hours apart do you take the second tablet. Is it as you state here (http://www.goutpal.com/gout-treatment/stop-gout/gout-attack/acute-gout-attack/) which mentions 1 tablet then a second 2 hours later or did you take 1 on the first sign of an attack and the other 12 hours later?
The reason I was initially asking was to see how many hours is a safe buffer for a first timer like me between taking the second tablet should I get an accute attack 🙂
-
August 2, 2017 at 10:16 am #4903
 Keith TaylorParticipant
Keith TaylorParticipantOIC @d_q
You’re the only person on the planet who takes any notice of my personal gout treatment program. And I include myself in that.
My reality is that I read stuff. Then, I talk to medical people about it if I get the chance. Next, I experiment within what I believe are safe boundaries to get a plan that works for me. So, with uric acid control, that’s easy. But with pain control, it’s more complicated. Especially with gout pain control.
First and foremost I had an epiphany when I realized gout pain stems from an immune reaction. Prior to that, I had the more typical view that sharp uric acid crystals were forming. So, I understood the importance of getting mobile as soon as possible. Fortunately, prescription strength ibuprofen (Aleve) kept me going almost every time. But if it didn’t I supplemented with paracetamol (Tylenol).
BTW, a quick aside, where are you buying your pain drugs? Diclofenac and naproxen are both widely available next to ibuprofen and paracetamol at your local Co-Op. I haven’t checked Aldi yet.
When I finally took some of my own advice and started allopurinol, my doctor brought colchicine into the mix as a preventative. Now, by this time, I understood how colchicine poisons the immune system to limit inflammation starting or spreading. So, I started preventative colchicine for two weeks every allopurinol dose change. Then as required.
So, the preventative part is not really part of this topic. But, I’ll explain it anyway because I think it’s where the 12 hours comes from. The best time to take preventative colchicine is at bedtime. But, if you wake up with slight gout symptoms, it’s usually the first sign of an attack. So, you prevent an acute attack with a morning colchicine. Also, consider a first NSAID at the same time. I used to wait a couple of hours before taking the NSAID, then realized I should be best taking them together. But remember I have absolutely no stomach effects, so you might need to carefully experiment.
Now, you might have a lazy 12-hour kip, d_q. But I’m happier with 5 to 8 hours. There is no fixed rule about hours. The second dose is backing up the preventative dose that might not have quite worked. It might not be necessary, but I’m not one to ask for an acute attack.
Returning to your acute gout attack plan. I have to say my advice is quite speculative. Because, since starting allopurinol, I have never had a serious acute attack. Though I have definitely experienced the onset of an attack and stopped it within 2 hours.
So, d_q, going back to your original “let’s say someone gets an acute flare today; what would be your dosing to hit hard?” My speculative answer was my “Dear Someone” letter above.
Finally, returning to the gap between colchicine doses.
Firstly, I’d suggest if you are worried, you switch to a different poison. Because there is always a risk of stomach problems with colchicine. Also, there are infection risks, so you have to be aware of germs from people around you.
If you do go down the colchicine route, I’m sure any doctor would back me up if I say you have to adjust your dose according to your personal experience. That means carefully recording your symptoms and reactions. An hour between doses should be OK. But everyone is different for all sorts of reasons.
I won’t bore you with all those reasons now. Instead, let’s look at the practical approach. The 2-hour cycle that I suggested above definitely works. I can’t think why you would want to take a second colchicine after only one hour, but it should not be a problem if the first one didn’t have you shitting yourself.
Thanks for helping me clarify this in my brain. Now, I need to review relevant pages to make sure all these points are covered properly. But first, I must worry about the grammatical challenges arising from my thoughts: “I can’t do this without d_q and nobody” 🙂
-
August 6, 2017 at 11:37 am #4950
d q
ParticipantOf course I take notice of your personal gout treatment plan 🙂
All the information you provide on the forum and publish on your site I thoroughly read. Ignorance is bliss but education is clarity.First and foremost I had an epiphany when I realized gout pain stems from an immune reaction. Prior to that, I had the more typical view that sharp uric acid crystals were forming. So, I understood the importance of getting mobile as soon as possible. Why was it important getting mobile as soon as possible when realising that gout pain stems from immune reaction?
I too am happy with 6-8 hours of sleep when possible 🙂 I was initially wondering what a safe buffer time between tablets was but now I understand the mechanism of timings from you and nobody’s excellent advice.
My rheumatologist suggested two preventative options for me, either 250mgs of Naproxen -or- 25mgs of Diclofenac for one week with every febuxostat increase or a month of colchicine when starting febuxostat.
My first attack was exactly 3 years ago and I cannot express just how much I want to be able to get on with life knowing this is all behind me.
p.s. Did you go to the USA..? 🙂
-
August 11, 2017 at 3:04 pm #5062
 Keith TaylorParticipant
Keith TaylorParticipantWhy was it important getting mobile as soon as possible when realising that gout pain stems from immune reaction?
Sorry @d_q, it’s taking me longer to answer that than I anticipated. The science (and my discovery of it) is on its way.
Also, I had a great time in the USA, thank you. So now I understand more about some of the different issues faced on each side of the pond. But, I didn’t get any time to research real practical issues. Like why Colcry$ remains popular when Mitigare is available.
-
-
August 15, 2017 at 10:26 pm #5194
d q
Participant@Keith – Good to hear you had a good time. I have USA on my visit list for next year. It’s probably going to be Italy for vacation this year 🙂
I’m extremely keen to read the article about getting mobile as soon as possible as I think I may have found a link to what I might be experiencing. Please let me know as soon as its ready for reading and where to look out for it.
Cheers mate.
-
January 19, 2019 at 4:31 pm #8790
 Antwerpen SevenParticipant
Antwerpen SevenParticipantMitigare for Gout prevention
Hi all,
I have reached the age at 54 where my gout attacks are increasing. I have been a gout sufferer since I was 30 but Prednisone quick 4 day doses were fine for the once or twice a year I to an attack. Now I am up to 6-8 times a year and my doc really wants me (as do I) on preventative meds.
My question is this: Few ever talk about it but I have seen that .6mg daily of Mitigare (colcochine) is actually an effective and good place to start for prevention and may be more effective than Alluprinol with less side effects and with good heart benefits. My doctor is not aware of this and wants me on Alluprinol. But I have read some things that Mitigare may be a better solution. I have used it before for a flare up and had no side effects so it’s also something I should be able to tolerate.
Does anyone have any experience with this as an alternative to the two more common preventatives?
-
January 19, 2019 at 5:44 pm #8791
nobody
ParticipantPeople have naturally talked about colchicine here. It’s by far the oldest gout medicine after all! It is not an alternative to allopurinol however. And the side effects of prolonged use are rather serious… colchicine is certainly not a drug you should take for years on end like allopurinol.
Gout does cause damage over the years if it’s not prevented so it’s unfortunate your doctor hasn’t insisted on allopurinol earlier.
The main alternatives to allopurinol are: lifestyle/diet changes and another drug called febuxostat. There’s also a class of drugs called uricosurics as well some herbal compounds and compounds found in common foods which are generally less effective. Finally, there’s a very powerful and expensive drug which is injected in the bloodstream. All in all, allpurinol isn’t a bad choice in most cases. There’s a genetic test to prevent bad reactions you can take if you have East Asian ancestry.
The point of allopurinol and its alternatives is to reduce the amount of uric acid in your body. Colchicine doesn’t do this. Uric acid is routinely measured and knowing the test results is helpful in narrowing down the best options for a particular gout sufferer.
Good luck!
-
-
-
AuthorPosts
The forum ‘Help My Gout! The Gout Forum’ is closed to new topics and replies.